Role of DOPAL in Parkinson's Diseases!!
Sunday, November 4, 2007
A team of scientists has announced proof that the chemical DOPAL starts the chain reaction that causes Parkinson's disease.
The St. Louis University researchers discovered that dopamine itself actually plays a role in destroying the cells that produce it. DOPAL is one of many possible residues that remains after dopamine is depleted. It happens to be a poisonous leftover.
Since the mid 1990s researchers have been trying to understand the impact of a chemical called DOPAL (short for endogenous metabolite 3,4-dihydroxyphenylacetaldehyde) on people with Parkinson's disease. This is the culmination of many years of research on the subject.
"The findings provide a target for Pharmaceutical companies and other researchers to block DOPAL formation and its toxic effects," wrote lead researcher William J. Burke MD, PhD, in an email to My Parkinson's info.
Scientists have long known that a key protein called alpha-synuclein plays a role in the development of Parkinson's disease.
Alpha-synuclein is found throughout the brain—but in some people, the protein clumps together. This causes the death of the dopamine-producing cells, which in turn causes Parkinson's to develop.
It is likely that these claims will meet some scrutiny from the scientific community, and the theories could be revised. We may learn that not all PD cases are caused by DOPAL. However, these findings should lead to some rapid research and development into better treatments for Parkinson's disease
After Brain Injury Stem Cells shown to improve Memory !!
New UC Irvine research is among the first to demonstrate that neural stem cells may help to restore memory after brain damage.
In the study, mice with brain injuries experienced enhanced memory -- similar to the level found in healthy mice -- up to three months after receiving a stem cell treatment. Scientists believe the stem cells secreted proteins called neurotrophins that protected vulnerable cells from death and rescued memory. This creates hope that a drug to boost production of these proteins could be developed to restore the ability to remember in patients with neuronal loss.
"Our research provides clear evidence that stem cells can reverse memory loss," said Frank LaFerla, professor of neurobiology and behavior at UCI. "This gives us hope that stem cells someday could help restore brain function in humans suffering from a wide range of diseases and injuries that impair memory formation."
The results of the study appear Oct. 31 in the Journal of Neuroscience.
LaFerla, Mathew Blurton-Jones and Tritia Yamasaki performed their experiments using a new type of genetically engineered mouse that develops brain lesions in areas designated by the scientists. For this study, they destroyed cells in the hippocampus, an area of the brain vital to memory formation and where neurons often die.
To test memory, the researchers gave place and object recognition tests to healthy mice and mice with brain injuries. Memories of place depend upon the hippocampus, and memories of objects depend more upon the cortex. In the place test, healthy mice remembered their surroundings about 70 percent of the time, but mice with brain injuries remembered it just 40 percent of the time. In the object test, healthy mice remembered objects about 80 percent of the time, while injured mice remembered as poorly as about 65 percent of the time.
The scientists then set out to learn whether neural stem cells from a mouse could improve memory in mice with brain injuries. To test this, they injected each mouse with about 200,000 neural stem cells that were engineered to appear green under ultraviolet light. The color allows the scientists to track the stem cells inside the mouse brain after transplantation.
Three months after implanting the stem cells, the mice were tested on place recognition. The researchers found that mice with brain injuries that also received stem cells remembered their surroundings about 70 percent of the time -- the same level as healthy mice. In contrast, control mice that didn't receive stem cells still had memory impairments.
Next, the scientists took a closer look at how the green-colored stem cells behaved in the mouse brain. They found that only about 4 percent of them turned into neurons, indicating the stem cells were not improving memory simply by replacing the dead brain cells. In the healthy mice, the stem cells migrated throughout the brain, but in the mice with neuronal loss, the cells congregated in the hippocampus, the area of the injury. Interestingly, mice that had been treated with stem cells had more neurons four months after the transplantation than mice that had not been treated.
"We know that very few of the cells are becoming neurons, so we think that the stem cells are instead enhancing the local brain microenvironment," Blurton-Jones said. "We have evidence suggesting that the stem cells provide support to vulnerable and injured neurons, keeping them alive and functional by making beneficial proteins called neurotrophins."
If supplemental neurotrophins are in fact at the root of memory enhancement, scientists could try to create a drug that enhances the release or production of these proteins. Scientists then could spend less time coaxing stem cells to turn into other types of cells, at least as it relates to memory research.
"Much of the focus in stem cell research has been how to turn them into different types of cells such as neurons, but maybe that is not always necessary," Yamasaki said. "In this case, we did not have to make neurons to improve memory."
Obesity more in brain than in your Food.
With nearly 30 percent of Indians suffering from obesity, people may be blaming their food habits.
But doctors in the capital Thursday said the real cause of this ailment lies in the brain. We are not giving a clean chit to food and lifestyle habits for this disease but metabolic activities in the brain is a major cause of this ailment.
Certain activities in the brain affect our genes and food intake. Due to this development, over 70 percent of intake calories get deposited in our body leading to problems like obesity and diabetes.
When a person becomes obese, it continues for at least the three next generations.If a person acquires obesity by himself without any contribution from his forefathers, then his next three generations will suffer from the ailment.
New medical procedures like surgery, stem cell therapy, gene therapy, insulin inhaler and other upcoming cheap but efficient drugs to tackle obesity and diabetes problems will be discussed at the conference. Health experts said currently nearly 30 percent of Indians are overweight and at least 50 percent of the country's population will suffer from this problem in next one decade.
Obesity is no more a disease of the adult and male population. Females and minors are getting affected by it too. While 57 percent of obese people suffer from Type-2 diabetes, 30 percent face gallbladder diseases, 14 percent osteoarthritis, 17 percent face hypertension and cardiovascular diseases. Some also face problems like uterine and breast cancer.
The problem is obesity leads to many health hazards and at one time a single individual may face a number of ailments. For every one diabetes case diagnosed in our country, two cases go undiagnosed and four cases have intolerable glucose level, which means they are on the verge of getting diabetic.
Now We Indians can afford Stem Cell banking too !!
Wednesday, October 31, 2007
Anand Mani, a pathology test vendor, wanted to gift his unborn child something special and his heart was set on saving the baby's stem cells for a disease free future. But the process was expensive.
Mani's dream may not have come true but for a new EMI (equated monthly instalments) payment plan.'I wanted to bank my child's stem cell. If I hadn't been able to do it for want of money I would have felt guilty lifelong,' Anand, now the father of a girl child, told IANS.
Stem cells are normally found in bone marrow and umbilical cords. They are the master cells responsible for producing all the mature cells in our blood and immune system. They form the white cells that fight infection, the red cells that carry oxygen, the platelets that promote clotting and the cells of our immune systems.Stem cells can be used for the treatment of Parkinson's, Alzheimer's, diabetes, leukaemia and 74 other diseases, which destroy the body's healthy cells.
The cost of harvesting, processing and storing stem cells is about Rs. 35,000 ($850) but this is too expensive for the common man.That is why stem cell bank Cryobank International is now offering a first payment option of Rs. 8,500 ($200) to store cord cells. The remainder is collected as EMIs of Rs. 3,000 ($75) and the EMI period can be stretched to 11 months or even 21 years.Such schemes have made it possible for people from low-income groups like Mani to access the path-breaking technology.
Pathologist Chaitanya V. Nerikar, chief executive of Cryobank International, told IANS that stem cell therapy was fast becoming an option for the common man in India.'And it will become cost-effective as more people go for umbilical cord cell banking,' she said.
There are 150,000 blood cancer patients in India. 'Complete change of blood has been the standard treatment worldwide for leukaemia but in India this is still not easily available because there is no national registry for matching blood,' Nerikar said.
In the West, such registries are available online.
New RNA Molecule could impact gene function
U.S. scientists determined a newly discovered class of tiny molecules of ribonucleic acid, or RNA, have a significant impact on gene function.
The Yale University Stem Cell Center researchers demonstrated for the first time a type of RNA called piwi-interacting RNA, or piRNs, performs crucial functions in controlling stem cell fate and other processes of tissue function serving as regulatory proteins.
Professor Haifan Lin, director of the stem cell center, heads the laboratory that originally identified piRNAs.
"These small RNAs might provide new tools to harness the behavior of stem cells and other biological processes related to diseases," said Lin. "This finding revealed a surprisingly important role for piRNAs Â… in stem cell division. It calls upon biologists to look for answers beyond the 1 percent of the genome with protein coding capacity to the vast land of junk (non-coding) DNA, which constitutes 99 percent of the genome."
The research is detailed in the journal Nature.
Stem Cells for damaged eyes and rare skin disorders
Thursday, October 25, 2007
http://www.eurekalert.org/pub_releases/2007-10/es
Doctors and scientists in Italy have shown how stem cells can be used to treat damaged eyes and, in combination with gene therapy, a rare and debilitating skin disease.
Professor Michele De Luca of the University of Modena and Reggio Emilia described the work to an international meeting of stem cell scientists in Milan (30 Sep – 2 Oct, “Challenges in Stem Cell Differentiation and Transplantation”) organised by the European Science Foundation’s EuroSTELLS stem cell programme in conjunction with the National Research Council of Italy.
Stem cell therapy involves the use of stem cells – ‘blank’ cells (‘toti- or ‘pluripotent’) that have not differentiated into specialised cells – to generate new tissues or organs. While widespread stem cell therapy lies some way in the future, Professor De Luca pointed out that it has been used already for many years in the treatment of burns. Many tissues of the body are continuously regenerated by their own population of stem cells. In the skin, such cells are called holoclones and for decades doctors have taken small samples of these cells from burns patients and cultured the cells into new skin that can be grafted onto the wound.
Professor De Luca’s team showed that cells of the transparent outer covering of the eye, the cornea, are constantly being replaced by new cells deriving from an area surrounding the cornea called the limbus. The cells differentiate into corneal epithelium and migrate to the cornea.
“If the cornea is damaged severely by a chemical burn or infection, for example, it can become opaque and necessitates a transplant,” Professor De Luca told the meeting. “However, a transplant will only be successful if the patient’s limbus has remained intact so that it can continue to replenish the new cornea.”
For many years doctors did not understand why some transplants failed – because they did not appreciate the requirement for the limbus.
In cases where the limbus is destroyed there has been little hope to restore the patient’s sight. Professor De Luca’s team decided to take a leaf from the way that burns are treated and grow a new cornea from limbar stem cells taken from the healthy eye.
By removing a small sample of these cells it was possible to culture a new cornea and graft it on to the damaged eye. The team showed that of 240 patients who were operated on in this way, the cornea regenerated successfully in 70% of cases.
The researchers then turned their attention to a rare but debilitating genetic disease of the skin resulting in a syndrome known as Epidermolysis Bullosa, in which the skin is highly fragile and prone to blistering due to faulty proteins that effectively anchor the surface layers of skin to the body.
In one form of the disease there is a mutation in one of these anchoring proteins called laminin 5. The Italian researchers obtained consent to carry out a small-scale trial of a novel gene therapy using skin holoclones on one patient, a 37-year-old male, on small part of his body .
“Because the patient’s body was so badly affected it was difficult to isolate any stem cells from his skin,” Professor De Luca told the conference. “Most people have between seven and ten per cent of holoclones. Our man had none. Eventually we found a few in the palms of his hand and cultured them from a biopsy.”
The team then used gene therapy to insert the correct laminin gene into the growing cells and grafted the new tissue onto the patient’s body. The graft was successful and after several months the skin remained to all intents normal, without the blistering and flaking.
“This demonstrates that it is possible to use stem cells in gene therapy for genetic skin disorders,” Professor De Luca said.
Stem Cells from patient's fat used to grow nerves
Stem cells from a patient's fat may be used to create new nerves that can repair severed peripheral nerves (nerves outside the spinal cord), say scientists from Manchester University, England. The researchers say this route for creating new nerves could be part of medical practice by the year 2011.
The scientists said their aim is to put the new nerve tissue inside a biodegradable plastic tube, insert in at the broken ends of the severed nerve, and rejoin them in a human. This procedure could help a considerable number of people. They say they have had promising results with rats.
Current medicine offers very limited procedures to help restore peripheral nerves. Nerves from elsewhere can sometimes be used- however, the risk of additional damage is significant, and even when there are results they hardly ever restore perfect function, say the authors.
The team managed to extract stem cells from the fat tissue of rats, and tweaked them to become neurons in the lab. Their aim now is to do the same, but with stem cells that come from human fat. They plan to create a replacement nerve, place it in a biodegradable sheath, and attach it to the severed part of the nerve. The result would be that the severed nerve would be joined again.
If successful, this technique could be used in any part of the body.
"The differentiated stem cells have great potential for future clinical use, initially for treatment of patients with traumatic injuries of nerves in the arms and legs," said team leader. As a study to find out how effective the biodegradable tube is is now being carried out, he believes we could be about four years away from an effective treatment for severed peripheral nerves.
Severed nerves can be caused by an accident, as well as surgery - a surgeon in his/her attempt to remove a large tumor may have to cut and damage nerves in order to do so.
Important Facts about HIV/AIDS
Tuesday, October 16, 2007
Causative agent:
HIV (Human Immunodeficiency Virus) is an incurable virus, which can cause a life-threatening condition called AIDS (Acquired Immune Deficiency Syndrome).
A person who has been infected with HIV is said to be HIV-positive.
There are two main types of HIV: HIV-1 and HIV-2. The most aggressive form of the virus is HIV-1. It is a RNA virus called retrovirus. Infection with HIV-1, does not mean the person is suffering from AIDS. It takes a long time about 10 years to develop AIDS from HIV positive state.
If untreated, HIV can cause so much damage that the infected person's immune system no longer works properly. When this happens, the person is said to have developed AIDS.
AIDS:
Acquired immune deficiency syndrome or acquired immunodeficiency syndrome (AIDS or Aids) is a collection of symptoms and infections resulting from the specific damage to the immune system caused by the human immunodeficiency virus (HIV) in humans, and similar viruses in other species (SIV, FIV, etc.). The late stage of the condition leaves individuals susceptible to opportunistic infections and tumors. Although treatments for AIDS and HIV exist to decelerate the virus' progression, there is currently no known cure. HIV,
Site of Action:
HIV differs from other viruses in that it specialises in attacking the very immune cells - white blood cells known as Helper T cells, or CD4 cells - that are designed to rid the body of infections.
By infecting and ultimately destroying Helper T cells, HIV seizes control of the body's immune system. Infected cells no longer behave as they should and instead of helping to fight the disease, they actually spread it.
Modes of Spread:
The most common ways that people become infected with HIV are:
* by having sexual intercourse with an infected partner
* by injecting drugs using a needle or syringe which has already been used by someone who is infected.
HIV can be passed on in both these ways because the virus is present in the sexual fluids and blood of infected people. If infected blood or sexual fluid gets into your body, then you can become infected.
Vaginal sex
HIV is found in the sexual fluids of an infected person. For a man, this means in the fluids which come out of the penis before and during sex. For a woman, it means HIV is in the fluids produced by the vagina before and during sex to help make intercourse easier.
If a man with HIV has vaginal intercourse without a condom, infected fluid can pass into the woman's blood stream through a tiny cut or sore inside her body. Such a cut or sore wouldn't always be visible, and could be so small that the woman wouldn't know about it.
If a woman with HIV has sexual intercourse without a condom, HIV could get into the man's blood through a sore patch on his penis or by getting into the opening that runs down the penis.
If there is any contact with blood during sex, this increases the risk of infection. For example, there may be blood in the vagina if intercourse occurs during a woman's period.
Oral sex
Oral sex with an infected partner does carry some risk of infection. If a person sucks on the penis of an infected man, for example, infected fluid could get into the mouth. The virus could then get into the blood if you have bleeding gums or tiny sores or ulcers somewhere in the mouth.
The same is true if infected sexual fluids from a woman get into the mouth of her partner.
But infection from oral sex alone seems to be very rare, and there are things you can do to protect yourself.
Anal sex
If a couple have anal intercourse the risk of infection is greater than with vaginal intercourse. The lining of the anus is more delicate than the lining of the vagina, so it's more likely to be damaged during intercourse, and any contact with blood during sex increases the risk of infection. Injecting drugs
Blood transfusions
Some people have been infected through a transfusion of infected blood. These days, in most countries all the blood used for transfusions is now tested for HIV. In those countries where the blood has been tested, HIV infection through blood transfusions is now extremely rare.
Mother to child transmission
An infected pregnant woman can pass the virus on to her unborn baby either before or during birth. HIV can also be passed on during breastfeeding.
If a woman knows that she is infected with HIV, there are drugs that she can take to greatly reduce the chances of her child becoming infected.
Infection in the health-care setting
Some health-care workers have become infected with HIV by being stuck with needles containing HIV-infected blood. A very few have become infected by HIV-infected blood getting into the health-care worker's bloodstream through an open cut or splashes into a mucous membrane (e.g. eyes or the inside of the nose).
There have only been a few documented instances of patients becoming infected by a health-care worker.
Tattoos / piercings
Anything which allows another person's body fluids to get inside your body is risky. If the equipment is not sterile, having a tattoo done could carry a very small risk.If you are thinking of having a tattoo or piercing, ask staff at the shop what procedures they take to avoid infection.
Kissing
At the moment, scientific opinion is pretty clear that you cannot become infected with HIV through kissing.
To become infected with HIV you must get a sufficient quantity of HIV into the bloodstream. Saliva does contain HIV, but the virus is only present in very small quantities and as such, cannot cause HIV infection.
Unless both partners have large open sores in their mouths, or severely bleeding gums, there is no transmission risk from mouth-to-mouth kissing.
Sneezing, coughing, sharing glasses/cups, etc
HIV is unable to reproduce outside its living host, except under very extreme laboratory conditions. HIV does not survive well in the open air, and this makes the possibility of this type of environmental transmission remote. In practice no environmental transmission has been seen.
This means that HIV cannot be transmitted through spitting, sneezing, sharing glasses or musical instruments.
You also can't be infected in swimming pools, showers or by sharing washing machines or toilet seats.
Insects
Studies conducted by many researchers have shown no evidence of HIV transmission through insects, even in areas where there are many cases of AIDS and large populations of insects such as mosquitoes. Lack of such outbreaks, despite considerable efforts to detect them, supports the conclusion that HIV is not transmitted by insects.
Also, HIV only lives for a short time and does not reproduce in an insect. So, even if the virus enters a mosquito or another sucking or biting insect, the insect does not become infected and therefore cannot transmit HIV to the next human it feeds on or bites.
Protected sex
If an unbroken latex condom is used, there is no risk of HIV transmission. There are myths saying that 'some very small viruses can pass through latex' - this is not true.
Anal sex is not necessarily a risk if unbroken condoms are used and there is no blood-to-blood contact. You can't 'create' HIV by having anal sex.
Although sophisticated laboratory techniques are able to isolate the HIV virus from other body fluids of infected people (such as saliva and tears) the level of virus in these fluids is far too low to be considered infectious.
Situation in India
India has among the highest number of persons living with HIV/AIDS in the world today, although the overall prevalence remains low. Some states experience a generalized epidemic with the virus transmitted from high-risk groups into the general population. A major challenge is to strengthen and decentralize the program to the state and district levels to enhance commitment, coverage and effectiveness.
Find out Breast Cancer In your Mom's Hips
Wednesday, October 10, 2007
In a Recent Interesting Study, Researchers have found out that women whose mother have large and round hips have greater breast cancer risk, nearly 7 times more risk.
A woman's Hip size is a marker of the hormone estrogen production. Wide Round hips represent markers of high sex hormone concentrations in the mother, which increases daughter's vulnerability to breast cancer.
According to the study, measurement taken was intercristal diameter, which is the distance between the top most points of the hip bones of the 2 sides. They found out the risk of Breast cancer increased to 60% in mothers who had hips more than 30cms across.
They also added that babies carried by wide hipped women for full 40 weeks of pregnancy or more had 3.7 times of risk of breast Cancer.
True human Tail !!
Monday, October 8, 2007
The Birth of a child with a caudal appendage resembling a tail is a very rare abnormality and generates an unusual amount of interest, excitement and anxiety
(1). True human tail is a rare event with fewer than 40 cases reported in the literature
(2). It is defined as a caudal, vestigial, midline protrusion with skin covering a combination of muscle and adipose tissue
Case Report
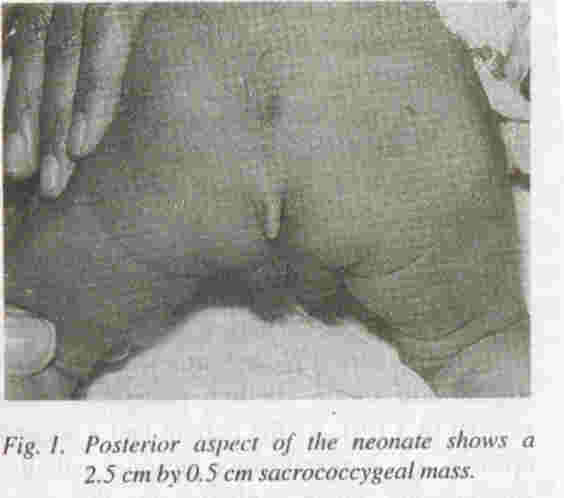
A 3 kg male Baby delivered was the product of full term pregnancy to 30 years old mother which was her 1st pregnancy, with no history of drug exposure during pregnancy or diabetes mellitus. The general and systemic examination of neonate was essentially normal except for tuft of hair in lower back (Sacrococcygeal) region in midline and a soft tissue tail like mass in the same region just below the tuft of the hair (see figure). Possibility of true neonatal tail verse's pseudotail was considered. The neonate did not have any other congenital anomaly. There was no family history of congenital anomaly. The soft tissue mass in the sacrococcygeal region was tail like, soft, well circumscribed measuring 2.5 cm by 0.5 cm. Radiography and ultrasonography of spine did not show any abnormality. This ruled out the possibility of spinal dysraphisam and parasite fetus (pseudotail).
For confirming the diagnosis of true tail, surgical excision of mass was planned, but very unfortunately it was not carried out as parents refused to give consent.
Discussion
Caudal appendages are unusual malformations and are divided into true tails and pseudotails (lipoma, teratoma, myelomeningocoele and parasitic fetus)(3). Simple surgical excision of true tail has been advocated(4). However, recent reports emphasize the associated midline anomalies that might change the surgical approach in these patients(5-7). It is important to make distinction between true and pseudotail in lumbosacaral region since the treatment and prognosis are different(2).
Pathogenesis & Etiology: remnant of embryonic tail. Fetal tail is a normal feature during embryonic development that should regress by the 8th week. Its persistence has been described beyond the 8th week.
Embryology: During the 5th-6th week, the human embryo has a tail with 10 to 12 vertebrae. Then, it starts to regress, reducing the number of vertebrae by fusion, leaving the vestigial coccyx. By this process, at 8 weeks, it disappears, although the exact moment varies. The persistent tail probably arises from the most distal non-vertebrate remnant of the embryonic tail.
Prenatal Diagnosis: Reported in a few cases.
Associated anomalies: spina bifida (20%), meningocele, lipomeningocele, chondrodysplasia, cleft palate, cutaneous hemangiomas, syndactyly and oligodactyly .
Differential diagnosis: Spina bifida, caudal regression sequence and sacrococcygeal teratomas.
Recurrence: never described.
Management: If diagnosed prenatally, no alteration of management is advisable as, to date, no morbidity or mortality related events have been described in these cases. After birth, a thorough examination, which includes CT-scan or MRI is suggested in order to rule out subtle anomalies prior to surgical removal of the tail.
Cancer Recurrence Research
Friday, October 5, 2007
The tumor grows back, despite post-surgery radiation and chemotherapy.
Researchers have identified a new reason for such recurrences: cancer stem cells.
Like regular stem cells, lauded for their role in regulating the body and their potential to become cures for diseases, cancer stem cells can self-renew and morph into many types of cells, scientists say.
But instead of giving people a steady supply of blood, skin or vital organ tissue, they propagate cancer growth, a growing body of research suggests.The theory, studied by Kuo and other researchers at UW-Madison and elsewhere, could explain why tumors often return after being nearly wiped out by cancer treatments.
|
|
“We’re leaving the seeds of tumors behind,” Kuo said.
He invokes warfare imagery when describing the limitations of today’s cancer therapies.
“We’re trying to attack the whole country of the enemy, but we’re missing the command and control structures,” he said.
First identified in leukemia a decade ago, cancer stem cells have since been found in brain, bone and other cancers. It’s not clear how the cells arise, but they may take shape when regular stem cells acquire certain DNA mutations, Kuo said.
If more research better defines cancer stem cells, new drugs might be developed to target and kill the cells, said Caroline Alexander, a UW-Madison researcher who studies the cells in breast cancer.
The theory also could lead to a radically new way of measuring the success of cancer therapy.
Instead of assessing how much of a tumor has been destroyed, doctors might try to find out how many cancer stem cells remain.
“If this is true, it will revolutionize oncology,” Alexander said.
But much work remains to be done, she said. “It’s a good idea still waiting to be demonstrated.“
They're studying if the cancer stem cells express different genes and signals in response to the treatments. Such markers could be targets for new drugs. Studies are going on to find out, why these cells are less sensitive to radiation and chemotherapy than the tumor they came from.
Continous Levodopa Therapy for Parkinson's Disease
Since many years, Doctors have wondered whether direct supply of levodopa and carbidopa to the intestines would give optimal effect. They have found out that the patients undergoing continuous levodopa therapy experienced a "heightened therapeutic effect, including a reduction in motor fluctuations.
Now , the medication called duodopa, administered into an area of the small intestine called the duodenum, is still in clinical trial in the United States. Using a small patient-controlled pump, the drug is continuously delivered through a tube that ends in the upper small intestine where it is rapidly absorbed. Some patients use a tube that travels through the nose, throat, and stomach, while others have the tube inserted surgically through the abdominal wall. Patients load the pump with a gel that contains levodopa and carbidopa. This delivery system ensures a more even supply and uptake compared with the conventional tablet treatment.
Duodopa administered as continuous levodopa therapy has shown remarkable results in people with advanced Parkinson's disease. Among the most optimistic reports, some people who were previously bedridden were able to walk again and use ability they had lost.
Hopefully this therapy makes its way through clinical trials quickly for people in the United States. It appears to have considerable potential to help people with Parkinson's disease. It has also been in practice in India by many neurophysicians. The response has been quite variable.
Stem Cells can trigger Cancer spread!
Thursday, October 4, 2007
Your body's own stem cells could trigger alterations in cancer cells which facilitate their spreading around the body. Scientists have found that human breast cancer in mice have a higher chance of spreading if they are blended with bone marrow stem cells. Fortunately, say the scientists, it is perhaps feasible to reverse the process, undermining the deadliness of the cancer.
When metastasis occurs it is much harder to treat the cancer. Metastasis is when the cancer invades other parts of the body and forms new tumors. In this study, the scientists intended to find out whether it was possible to stop this from happening - they wanted to find a means of isolating the cancer to one part of the body; stopping it from metastasizing (spreading, invading other parts).
The researchers have found an association with a specific type of stem cell, which encourages the breast cancer cells to spread to other parts of the body. They are found in the bone marrow, and are called Mesenchymal stem cells. These stem cells generally turn into cartilage, bone fat and muscle.
Previous studies had indicated that these stem cells generally migrated in huge numbers to where tumors were situated, meaning they were probably involved in the spread of the cancer. The researchers mixed these stem cells with human breast cancer cells in mice and found they spread to the lungs at seven times their normal rate.
The scientists believe the stem cells alter the cancer cells so that they metastasize. However, they add that as soon as they had spread, those cancer cells returned to their original genetic make-up. The bad news here is that as they revert back to their original genetic make up they are hard to identify, the good news, say the researchers, is that it is most likely they can find a way of blocking the whole process.






